This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to the Curbsiders. I'm Dr Matthew Watto, here with my great friend, Dr Paul Nelson Williams. We're going to recap some top pearls from a recent podcast, Adrenal Incidentalomas with Dr. William Young, who is a fantastic expert. To start us off, what should we think about when a patient has an incidentaloma? What are the first questions we should ask?
Paul N. Williams, MD: The first question, when you find something that shouldn't be there, is whether it's malignant or benign. You can reassure yourself to some extent that most aren't malignant, but even the benign mass could be hormone-producing, which is the second question. So, your two questions after finding an adrenal mass are 1) should this scare me, and 2) is this adenoma producing hormones that could adversely affect the patient?
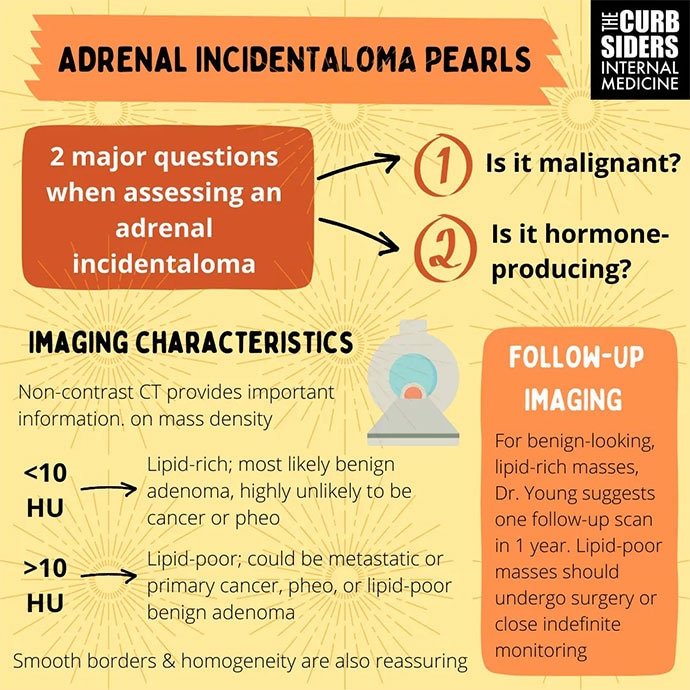
Watto: I loved his comment about imaging. When an adrenal mass is discovered incidentally, the original imaging might not give much information, such as whether it's lipid-rich or lipid-poor. They're not giving you the Hounsfield units (HFU), which Dr Young thinks are important.
A lipid-rich adenoma is usually < 10 HFU. That's very reassuring that it's not malignant. It's not a pheochromocytoma. In this case, you are thinking about subclinical Cushing syndrome or an aldosterone-producing mass.
For adenomas that are > 10 HFU, you're thinking that it could be a pheochromocytoma or a malignancy, which will lead you down a different pathway. But in primary care, the majority of the time, if we're going to do any preliminary workup ourselves, we can look for subclinical Cushing's or primary aldosteronism. Were you familiar with subclinical Cushing's? This was
a totally new concept.
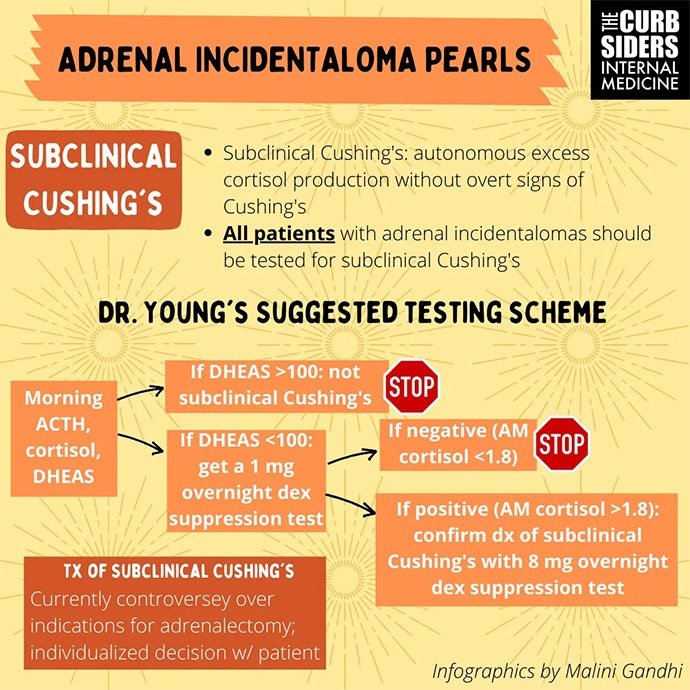
Williams: Exactly the same. When I hear "benign," I'm like, whew — I'm done. But Dr Young taught us that these functioning nodules — and this is how he frames it when talking to patients — are like getting a daily dose of prednisone, with all the adverse effects you might expect over time. So even though it's "benign," there is still biochemical activity that can lead to worse glucose control, osteoporosis, or hypertension. You still owe the patient a workup because it might be something you can intervene upon or somehow change your management of the patient.
Watto: Subclinical Cushing's means they don't have the moon face, the buffalo hump, or the purple striae. But when you do the biochemical workup, it's positive. And he said it's the equivalent of getting 5 mg of prednisone a day, which is not something you would ever do for no reason.
He likes to start with a two-step test. You check baseline active cortisol and dehydroepiandrosterone (DHEA) sulfate levels. If the DHEA sulfate is > 100 µg/dL, it's probably not subclinical Cushing's. They are making enough DHEA sulfate to prevent everything being shunted toward the cortisol pathway. If the DHEA sulfate is < 100 µg/dL, he would try to see if he can suppress the patient's cortisol production with a 1-mg dexamethasone suppression test. Two days are required because you have to wait until the next day to check the cortisol level.
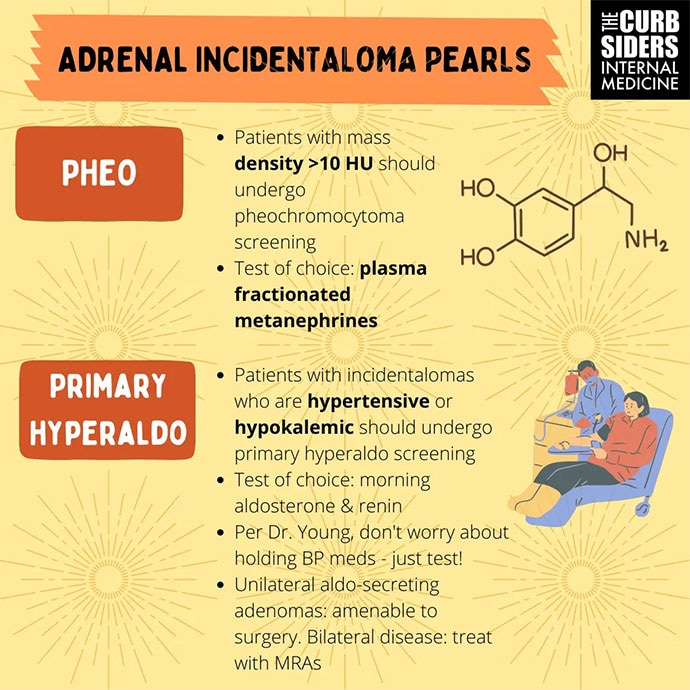
He also said that primary aldosteronism is very common. He thinks all patients with high blood pressure should be tested for it at least once because it's underdiagnosed. For people with an incidental nodule, he recommends checking early-morning aldosterone and renin, and if the renin is suppressed and the aldosterone level is ≥ 10, you should think about primary aldosteronism.
We go into more details on the full podcast about what to do if you find an adrenal incidentaloma. Anything to add, Paul?
Williams: If this all sounds good to you, you should check out the full episode here.
Watto: We talk about treatment. We talk about the next lines of testing and which people are going to need their adrenal activity done to try to fix this problem.
Until next time I'm Dr Matthew Frank Watto.
Williams: And I remain Dr Paul Nelson Williams Thank you and goodbye.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Credits:
Images: The Curbsiders
© 2023 WebMD, LLC
Cite this: Matthew F. Watto, Paul N. Williams. Finding an Adrenal Incidentaloma: What to Do Next - Medscape - Apr 20, 2023.












Comments