Failed Fertilization: Is Genetic Incompatibility the Elephant in the Room?
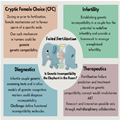
A recently published opinion paper by Dr Jukka Kekäläinen hypothesized that cryptic female choice (CFC), i.e. female-driven mechanisms that act primarily prior to or during fertilization and bias it towards the sperm of specific males, could also be involved in human fertilization (Kekäläinen, 2021). As the human species is labelled inefficient with regards to reproduction and the success rate of ART has not increased in the last decades (Gleicher et al., 2019), the idea that gamete compatibility could be the missing puzzle piece to complete our understanding of the intricate process of fertilization and partly explain the phenomenon of fertilization failure, is fascinating. Kekäläinen (2021) focused on evolutionary genetics in animal reproductive physiology and rationalized the hypothesis of gamete compatibility in humans, but did not elaborate on the possible clinical consequences of his theory. Defining the potential clinical relevance of genetic compatibility is an ambitious undertaking and one which led to a multidisciplinary discussion involving experts in evolution, genetics and reproductive medicine at the live edition of the ESHRE Journal Club at the 38th ESHRE annual meeting (see Figure 1 for a graphical summary of the main points of the discussion).
Figure 1.
Graphical summary of the #ESHREjc discussion.
Reproductive isolation, the process by which different species or specific populations can no longer reproduce with each other, is the strongest form of reproductive incompatibility found at the level of species or populations. Specific postcopulatory or prezygotic mechanisms relating to gametes may be at play and have been studied mainly in species with external fertilization such as the various dipteran species of Drosophila in the Caribbean. Island populations of these flies have evolved in a geographically isolated fashion, giving rise to particular subspecies that are still partially able to interbreed (Wilder and Hollocher, 2003). Interestingly, Drosophila arawakana and Drosophila nigrodunni crosses showed that D. arawakana males were unable to fertilize D. nigrodunni females' eggs. The females of such matings had a swollen reproductive tract containing fewer sperm (Hill et al., 2021), an example of postcopulation incompatibility. Hill et al., identified variants of genes encoding proteins for seminal fluid, copulation, stress and immune response, which are likely involved in gamete recognition and CFC. While these results are unlikely to be directly relevant to human reproduction, they do set the scene for the type of interactions that may be critical in genetic incompatibility. However, for Homo sapiens, relatively young species, such genetic differences in gamete recognition are both less likely and trickier to identify. Hence, we are still unable to fully explain failed fertilization in humans. In his article, Kekäläinen puts forward the idea that it is unlikely for failed fertilization to occur due to the deletion of genes involved in gamete recognition on eggs and sperm. Instead, he suggests that different alleles of the genes involved coevolve rapidly, and may therefore become incompatible, contributing to failed fertilization.
The concept of absolute or partial gamete compatibility or incompatibility in a couple is new and, if corroborated, could indeed redefine infertility. The only known form of incompatibility with a genetic cause in humans is linked to consanguinity, resulting in miscarriages and malformations due to an increased rate of homozygotes for autosomal recessive disorders (Tadmouri et al., 2009). We do not know if there are forms of incompatibility that directly prevent or hamper fertilization in a specific couple. At the molecular level, one key pair of genes essential for human gamete recognition and fusion are the JUNO (egg) and IZUMO (sperm) genes (Inoue et al., 2005; Bianchi et al., 2014). During the discussion at live #ESHREjc, it was emphasized that sperm and eggs produced by a single human follow Mendelian genetics in the assortment of alleles, resulting in half of the gametes carrying one allele variant or the other in a heterozygous individual. Although it has been clearly established that single mutations hamper Juno-Izumo binding and this can affect fertilization in mice and humans (Bianchi et al., 2014; Ohto et al., 2016), it is not known whether there are some JUNO allele variants that could be incompatible only with some specific IZUMO allele variants and not others, selectively preventing successful fertilization in a specific couple or among some gametes of that specific couple. Similarly, we do not know the potential role of mutations that affect other proteins essential for fertilization, such as MAIA that forms a highly stable interaction with the Izumo/Juno sperm-egg complex, permitting specific gamete fusion (Vondrakova et al., 2022).
If we accept the notion that evolution and molecular gamete recognition may drive genetic (in)compatibility during fertilization in humans, the next question would be whether this could influence clinical practice? Current technologies already help alleviate some types of incompatibility. For instance, incompatibility related to female reproductive secretions is circumvented with conventional IVF, while incompatibility of membrane-bound factors during fertilization is overcome with ICSI. In our efforts to combat infertility using these medically assisted reproduction technologies, do we disrupt nature by allowing fertilization of incompatible gametes? In the last two decades, the indications for IVF have expanded considerably beyond its initial application for tubal infertility (Kamphuis et al., 2014). Does the use of techniques out with their original indication, such as ICSI for non-male factor infertility (Haddad et al., 2021) risk interfering with human evolution? Although this is not an easy question to address, the relatively small contribution from IVF and ICSI towards all births makes this unlikely, at least from a genetic incompatibility perspective. In Australia, for example, IVF/ICSI babies make up <5% of all babies born (Choi et al., 2022), while the most common cause of infertility and ART use is delayed childbearing (Lambalk, 2022), which would not be related to genetic incompatibility. The next question, directly correlated to the possibility of gamete incompatibility in humans, is how applicable this information is in terms of diagnostics and, importantly, treatment. For diagnostics, a hypothetical pipeline to assess the allele distribution in patients in terms of receptor binding affinity could involve tools such as genetic screening, generation of cell surface protein structure models and in silico protein binding affinity prediction. We are certainly not there yet, but such avenues have the potential to revolutionize clinical practice, especially in cases of idiopathic infertility. For example, total fertilization failure occurs in 5–15% of IVF cycles (Barlow et al., 1990; Bhattacharya et al., 2001) and in 2–3% of ICSI cycles (Flaherty et al., 1998; Bhattacharya et al., 2001; Esfandiari et al., 2005). These cases would be the most immediate candidates to explore the diagnosis of gamete incompatibility. However, also in cases when there is suboptimal fertilization, a form of genetic incompatibility on a single gamete level cannot be completely ruled out. The challenges around designing genetic screening tests on a gamete level and treatment concepts are many. Identification of functionally important genes responsible for gamete level incompatibility and the development of analytical methods for genome-wide characterization of their interactions will be laborious and not necessarily straightforward. With increased cost-effectiveness of genomic testing and availability of gene panels for genetic causes of infertility, expanded carrier screening may become one of the options. However, the implementation of reliable clinical tests for parental genetic compatibility will not be simple from a methodological and ethical perspective (de Wert et al., 2021). When it comes to treatment, if gamete level incompatibility is found to cause a proportion of infertility cases, we would have the moral obligation to provide treatment. But, what if a more invasive treatment, such as genome editing, would be required to treat these patients? At the live #ESHREjc discussion during ESHRE 2022, participants highlighted the need to identify mechanisms of gamete level compatibility, if they exist in humans, in a pre-clinical context, and to explore their role in idiopathic infertility before testing the safety and efficacy of any treatment options in a research setting. We also lack large association studies in humans regarding this type of infertility. But again, genome-wide studies may not be able to provide answers, since we are an evolutionary young species and no human populations are reproductively isolated. It is important to highlight that at the current stage, any talk of clinical use or commercialization is purely hypothetical, non-evidence based and thus, unethical.
We need to investigate the molecular mechanisms of human gamete interaction through collaborations between reproductive biologists, molecular geneticists and evolutionary biologists. Such studies have the potential to redefine unexplained infertility and to identify and manage individual genetic incompatibility. This may take the form of, for example, fertilization failure prediction testing prior to IVF and selection of compatible gametes for ICSI in the forefront of novel technologies that will widen the repertoire of available infertility treatments, revolutionizing the field. This process requires rigorous research planning, from bench to bedside, with a concurrent discussion involving bioethicists, scientists, clinicians, embryologists and patients.
Data availability
No datasets were generated or analysed in this article.
Acknowledgements
The authors thank the author of the discussed paper, Dr Jukka Kekalainen; the Editor-in-Chief of Human Reproduction, Prof. Nils Lambalk; and all the participants (both in person and virtual) of the ESHRE live journal club at the ESHRE 2022 Annual Meeting.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Hum Reprod. 2023;38(2):324-327. © 2023 Oxford University Press