This transcript has been edited for clarity.
Carolyn A. Chan, MD: Welcome back to The Curbsiders, addiction medicine. I'm Dr Carolyn Chan. And today I am really excited to be joined by my good friend and co-host, Dr Shawn Cohen. Shawn, how are you? What's up? What's new?
Shawn M. Cohen, MD: It feels weird to be on video. But I promise that no one watching will whine about this video.
Chan: Your pun is fitting because we're going to be recapping a podcast episode from our Curbsiders addiction medicine series, titled Get in the Spirit of Ambulatory Alcohol Withdrawal, with the wonderful Dr Stephen Holt from the Yale School of Medicine.
This is one of my favorite episodes that we've produced this season. Dr Holt took us through the risk factors and pathophysiology of alcohol withdrawal. People who are most at risk for withdrawal generally consume about four to six standard drinks every day for about a month. And people with prior history of alcohol withdrawal are at the highest risk of experiencing alcohol withdrawal again.
He led us through a great explanation of the pathophysiology. Alcohol essentially cools down the brain through GABA, and over time with chronic consistent use, our internal cooling system is downregulated and our glutamate system gets amped up. So, when alcohol is reduced significantly or stopped abruptly, our internal cooling system is not working. This is what leads to alcohol withdrawal symptoms.
Shawn, would you tell us a little bit more about what this looks like in clinical practice?
Cohen: I love that analogy. It really helps me think through alcohol withdrawal and it guides both the symptoms and the treatment. We generally think about alcohol withdrawal symptoms in two buckets: mild to moderate symptoms; and then the severe, really scary things that can lead to morbidity and mortality. Truthfully, it's a spectrum. The mild symptoms are those that pop up within the first couple of days among people withdrawing from alcohol: nausea, gastrointestinal upset, tremors, anxiety, headaches, a skin-crawling feeling, being sweaty. A subpopulation of patients also experience hallucinations related to alcohol withdrawal, but they know they are hallucinations. They are alert, awake, and aware.
I think of these mild symptoms as being caused by too little GABA, that internal cooling system. On the other side of the spectrum is severe alcohol withdrawal. This is the minority of patients, less than 5%. But if you practice mainly in the hospital, you probably think it's a lot more common. These are people who have delirium tremens, meaning they become delirious, with a waxing and waning mental status. They have hyperactive adrenergic systems, so they have tachycardia and hypertension, and they can have seizures too, as early as 8 hours after stopping alcohol. But the rest of these symptoms begin around the 72-hour mark. We think of these as being both from too little GABA or from the brain overheating from too much glutamate, which leads to a hyperadrenergic state with too much dopamine.
Severe withdrawal is relatively uncommon. Patients with mild withdrawal symptoms can be safely managed in the outpatient setting. A big takeaway for me was how to triage these patients. How do we figure out who is safe to manage in the outpatient setting?
Chan: The foundation of person-centered treatment is the fact that most people really don't want to go to the hospital. It's not a fun place to be and it can be really stigmatizing for individuals with a substance use disorder. Ambulatory alcohol withdrawal management is safe. It can help us gain trust and it reduces hospital strain.
Dr Holt reviewed the absolute relative contraindications to ambulatory alcohol and drug withdrawal management.
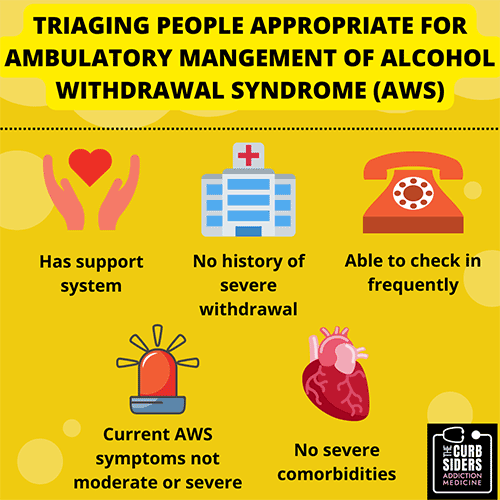
Figure 1.
Absolute contraindications include a history of severe or complicated alcohol withdrawal symptoms. These are patients who are having seizures and delirium tremens and they really need a higher level of care, or a patient who arrives at the clinic already having severe or complicated symptoms. Severely affected patients aren't going to be able to go to the pharmacy to pick up medications in a timely manner. They need to start treatment ASAP.
You have to use your clinical judgment. Comorbidities include congestive heart failure, decompensated cirrhosis, chronic kidney disease (stage 3 or higher), COPD, unstable psychiatric disease, and pregnancy. Patients with these conditions need additional monitoring as well as psychosocial support. This includes individuals who are living alone or have transportation barriers, and patients who have other substance use disorders or are taking sedating medications. Is the individual managing other active substance use disorders, or are they on any other sedating medications?
If the patient has any of these absolute or several relative contraindications, it's probably safer to recommend hospital-based treatment of their alcohol withdrawal. That being said, some patients will decline to go to the hospital for management, and for certain individuals it may be safer to trial a supervised ambulatory alcohol withdrawal management protocol rather than no medical care at all for their symptoms. Dr Holt made a great point that we should document the conversation around this. We discuss this carefully with our patients and we try to meet them where they're at.
Say we have a patient who doesn't have any of these contraindications and they say, "I want to give this a try." How would you talk to a patient about how we're going to do this?
Cohen: It's worth emphasizing the relative contraindications because many of our patients will have some of those. Having that discussion is about trying to do what's best for them. Maybe it's not hospital management.
The management of alcohol withdrawal comes right back to the pathophysiology we've talked about. Patients with mild or moderate symptoms of alcohol withdrawal have too little of that cooling system, too little GABA. To treat these patients, we need to replace the GABA in the brain, and the way we do that is with benzodiazepines and gabapentin.
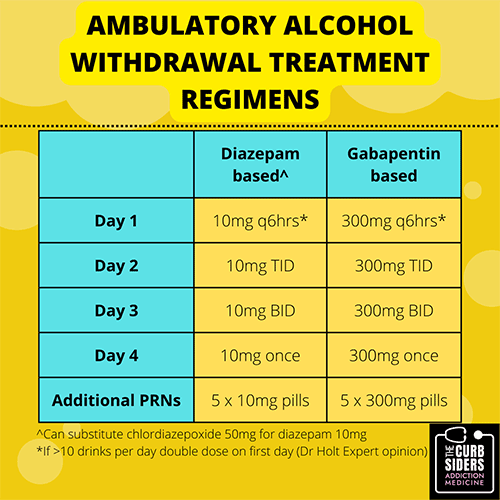
Figure 2.
These drugs replace the missing GABA. We slowly taper them off. We usually use longer-acting benzodiazepines to get symptom control. Diazepam or chlordiazepoxide are first line here because we have more data behind them than we have for gabapentin use in ambulatory alcohol withdrawal. Gabapentin has the added benefit that you can use it to treat alcohol use disorder as well.
For withdrawal, we generally use a 4-day taper with diazepam, starting with 10 mg every 6 hours. The next day it's taken every 8 hours, then every 12 hours and finally once per day. You give people a couple of pills to use as PRNs if they're having uncontrolled symptoms during the taper.
You also talk them through red flag symptoms such as being disoriented or confused or having a seizure. These are reasons to hospitalize them for treatment. For those doing the taper at home, we need to check in with them (ideally every day) to see how they're doing.
Another thing that can be very helpful is for the patient to have a support person, a partner or family member, or someone they live with who can watch them during this process. The support person can make sure the medicines are taken and make sure the patient is not getting confused. That person can be involved in the telehealth or other follow-up of the patient.
FinalIy, I would be a terrible addiction medicine doctor if I didn't emphasize that alcohol withdrawal is a symptom of alcohol use disorder. So you should use your opportunity of treating ambulatory alcohol withdrawal to also address the patient's alcohol use disorder. Medications are incredibly effective and we should be using those to treat alcohol use disorder, too.
Chan: To learn more about the pharmacology of alcohol use disorder treatment, you can check out our episode, Wrapping Our Heads Around Alcohol Use Disorder Meds.
We've tried to cover a lot in a brief period of time, and other nuances are important, so be sure to listen to the original podcast, Get in the Spirit of Ambulatory Alcohol Withdrawal.
As always, we're committed to high-value, practice-changing knowledge. To do that, we want your feedback. Please contact us here and let us know your thoughts about this podcast, or suggest other topics we should cover. Until next time, I'm Dr Carolyn Chan.
Cohen: I'm Dr Shawn Cohen. That's a wrap. Thanks for joining us.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
© 2023 WebMD, LLC
Cite this: DTs and More: Safe Outpatient Alcohol Withdrawal - Medscape - Jan 06, 2023.












Comments