This transcript has been edited for clarity.
Molly Heublein, MD: Hi. I'm Dr Molly Heublein. Welcome to Curbsiders TEACH, our Curbsiders family podcast on teaching in medical education.
Era Kryzhanovskaya, MD: And I'm Dr Era Kryzhanovskaya. We're excited to recap one of our favorite podcast episodes from Curbsiders TEACH season 2 — "Precepting Model Potpourri" with Dr Alaka Ray and Dr Ryan Nall.
Heublein: This was such a fun episode, and I got a lot of great pearls out of it. We review four different approaches to precepting in the clinical setting, the traditional precepting model, the 1-minute preceptor, SNAPPs, and precepting in the presence of the patients (PIPP). I love this episode because as an outpatient academic internist, I do a lot of precepting in clinic and hearing more approaches is always really helpful. Let's set the stage with thinking about the traditional precepting model. Era, could you describe what that looks like and when you might use it?
Kryzhanovskaya: The traditional model is one that many of us are familiar with. Perhaps it's even what we do. For many precepting encounters, the traditional model focuses on clinical supervision, making sure to provide the safest care for the patient. The learner presents information to the preceptor, the preceptor asks for additional details and then gives a plan to learner to implement as opposed to asking for their well-reasoned plan. Often, no deliberate teaching occurs. If teaching does occur, it's usually specific to the patient case and not really generalizable to future patient care. Typically, no direct feedback is given to the learner. Indirect feedback is provided as the preceptor does make changes to the care plan or presents their own care plan. This model is typically time efficient for patient care. However, it does not allow the preceptor to assess the learner's knowledge or their clinical reasoning skills. And while many of us are familiar with this approach, our Teach episode walks us through a few other approaches to precepting to consider. Do you want to explain the 1-minute preceptor approach?
Heublein: This is the first one that I was exposed to as a clinician educator, and I think it's a great one because it's so simple but also so practical and can really help up your teaching if you don't feel confident jumping into it without a framework. The 1-minute preceptor focuses on five micro-skills.
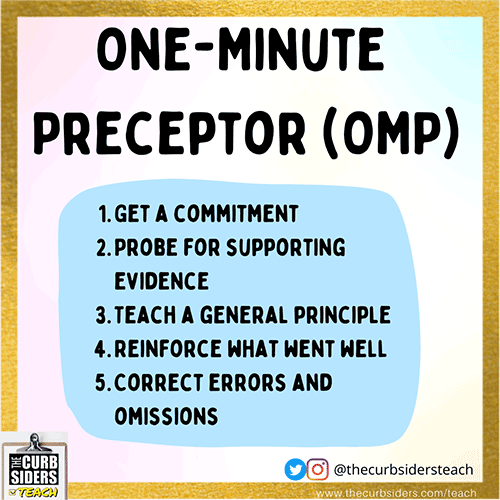
Figure 1.
Getting a commitment can be either a diagnosis or a next step in management. You really need to ask the learner what the working diagnosis is. If it's a clear diagnosis that's already established, what's the next step in treatment? Getting them to really put down their money, decide what they want to suggest, and commit to it. And then step two, you want to probe for supporting evidence. That's asking the learner questions about how they got to that point, how they got to that commitment, and what kinds of things support or discourage other clinical diagnoses. The goal here is to understand the learner's thought process and clinical reasoning so that you can really help them learn and grow. That leads us to step three, which is teach a general principle. This is a short, succinct teaching pearl that the learner can apply to future patient care. We're really busy in the outpatient setting. A quick pearl is really all the learner is able to take in and carry forward.
Step four is reinforce what went well — encouraging correct thinking patterns and illness scripts that are spot-on. Step five is correct errors and omissions and be mindful about the space in which you're providing the critical feedback. It may be best to save this for a one-on-one session rather than a crowded room, and for more advanced learners without errors in their presentation, you could ask about other differential diagnoses as a thought exercise to avoid anchoring. Ask, "What if the situation were a little bit different? Where would you take this?"
Kryzhanovskaya: I actually like to use the 1-minute preceptor model in presenting situations with early learners. It tends to be focused on making the diagnosis and what went into that process for the learner. So I like that we get to pause and have a discussion around the showing of the work or how learners got to a particular diagnosis, what they considered and what else went into their consideration.
Heublein: Let's talk about SNAPPS.
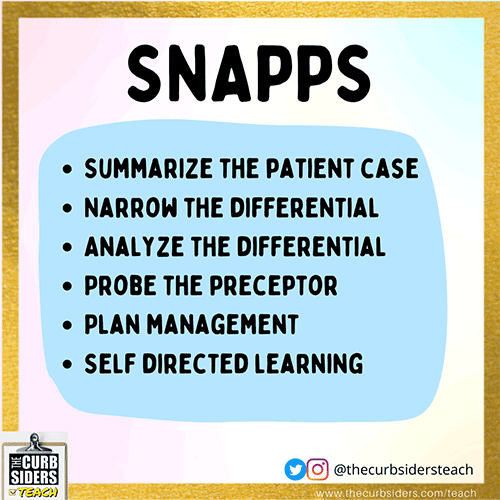
Figure 2.
SNAPPS is a great learner-driven approach, and it's really best in that sense for more advanced learners who can self-assess knowledge gaps. It forces the learner to identify the knowledge gap as a self-directed study at the end of this model, which is a key component of the strategy. This is a great one for learners who maybe work with preceptors who are more tied to that traditional model and maybe need to push their preceptor to help them learn a little bit more.
Kryzhanovskaya: I have deep thoughts about the SNAPPS model, but truly, I do like it. And I like that it gives a chance for the learner to do more self-directed learning and self-directed assessment.
Let's move on to our final model, the PIPP.
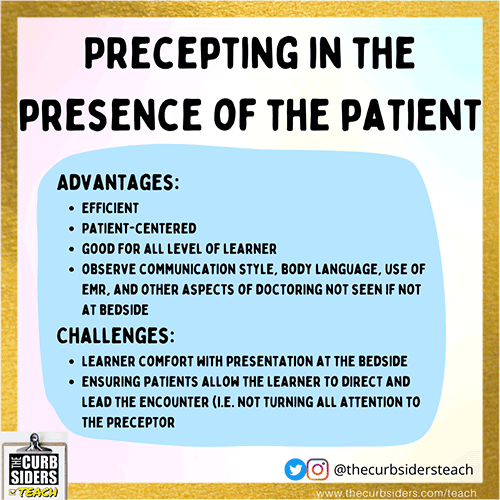
Figure 3.
This is the outpatient equivalent of inpatient bedside presentations. A learner stays and examines the patient as usual. When the learner is ready, the preceptor joins the learner in the exam room. So the presentation actually occurs in front of the patient, at which time the preceptor can ask clarifying questions, perform any additional exam maneuvers, and review the plan with the patient and the learner. The preceptor can also add teaching pearls in the exam room and if necessary, debrief with the learner after the encounter. This model is efficient. It is patient-centered. PIPP increases the face-to-face time with the patient and can actually reduce the patient's length of time in the office. This model works really well for early and advanced learners. It also allows the preceptor more time to observe the learner, especially in the exam room, and to provide feedback. Have that feedback conversation on the communication style, the body language, the use of the electronic health record, and other aspects of doctoring that are often not observed if you're receiving the presentation outside of the exam room. There are challenges, of course, to this presenting model, and they include making learners feel comfortable presenting in front of the patient and ensuring that the patient allows learners to direct the encounter as opposed to what might happen when the patient just directs all their attention to the preceptor.
Heublein: I have tried the PIPP model when we're running behind and just need to catch up a little bit on time. In that sense it can work really well to save time for the patient. Sometimes, our patients are waiting for an hour to see the resident. Anything that can improve efficiency for the residents is great.
Each of these precepting models allows the preceptor to assess the learner's thought processes and clinical reasoning, and that's key in our role as educators — to encourage our learners to grow and see where their learning edge is. With the traditional model, we don't have a sense of how much skill and knowledge they carry. And maybe we're teaching something that they already know and maybe we're not guiding them in the way that they need.
One thing that all of these models have in common is deliberate practice and intention. As long as you're deliberate and intentional, you can choose any precepting model or aspect of one of these models and make it work for you. You don't have to go through all five steps. You could just pick two and focus on those.
And there have been outcome studies from these different approaches. The one minute preceptor seems to be more focused on differentials and diagnostic evaluation as compared to the traditional model, which is more focused on history, taking risk factors and presentation skills. The SNAPPS model is more likely to explore differentials and justification for those as compared with the traditional model. So we have good data that these precepting approaches really do change the information that we hear from our learners.
Kryzhanovskaya: To add a few tips on teaching pearls, we often teach around differentials and medical knowledge, but you can, as a preceptor, also go into areas of management reasoning. If you want to learn more, see our season 1 episode, "Management Reasoning: What Is It and How Do We Teach It?" This is a chance for the preceptor to teach about processes. Some residents are super solid on their medical knowledge, but they have gaps around getting things done. Teaching on management reasoning can be generalizable and will empower residents, especially if that's who you're teaching, to take better care of their patients. This is the "getting stuff done" reasoning that is part of being a physician and part of excelling in systems-based practice with advanced learners. It can also be helpful to push their thinking with hypotheticals, as Molly mentioned earlier. So if someone is hitting the nail on the head with their presentation, maybe asking again, "What would you do if this patient had X, Y or Z," or "Why wouldn't this other medication work well in this situation?"
Heublein: We also had a great conversation about continuous improvement as a preceptor. One pearl that I loved from Drs Ray and Nall was that to improve feedback conversations with learners, it can be very helpful to have the attending start off by sharing something that they feel like they didn't do well or that they're trying to improve upon to allow the learners to feel comfortable sharing things that they feel like the attending could work on. It can help us get the feedback we need to improve our skills. It can also be very helpful to get your peers to sit and watch you or watch your peers to learn new approaches to teaching in clinic.
If you want to hear the full podcast, click on Teaching in the Ambulatory World: Precepting Model Potpourri (PIPP, SNAPPS, OMP). You can see our show notes and graphics there as well. I'm Dr Molly Heublein.
Kryzhanovskaya: And I'm Dr Era Khrzhanovsky. Thanks so much for joining us on this quick refresher of our preceptor models with Dr Alaka Ray and Dr Ryan Nall.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
© 2022 WebMD, LLC
Cite this: Molly Heublein, Era Kryzhanovskaya. Med Ed: How to Be a Better Preceptor - Medscape - Dec 22, 2022.







Comments